Regenerative Medicine for Orthopedic Conditions
In recent medical history, a focus on healing the body through more natural means has come to the forefront. Where traditional medicine has fallen short and continues to look for answers, a new type of medicine has emerged, Regenerative Medicine. Using the body’s own healing properties to focus in on injured tissue, regenerative medicine continues to steadily gain ground in health care.
Although broad by definition, regenerative medicine primarily involves two individual procedures, Stem Cell Therapy and Platelet-Rich Plasma Therapy (PRP). Both techniques focus on the concentration of a substance that targets injured or absent tissue. In orthopedics, these procedures have great promise for their use on injuries to bone, cartilage, muscles and tendons. These procedures have seen positive results in treating the shoulder, knee and other joints.
The rotator cuff is a group of four muscles that produces movement in the shoulder. The four muscles which include the supraspinatus, infraspinatus, teres minor and subscapularis, attach the scapula to the head of the humerus and provide movement and stability to the shoulder. The tendons form a capsule or a cuff around the shoulder joint providing structural support and functional movement.
Injury to the rotator cuff is a common condition of the shoulder that affects individuals from many backgrounds and activities. Injuries of these tendons are understood to impact 1 in 5 adults in their lifetime.1 Common injuries include: tears to the tendon, tendonitis and other tendonopathies.
and activities. Injuries of these tendons are understood to impact 1 in 5 adults in their lifetime.1 Common injuries include: tears to the tendon, tendonitis and other tendonopathies.
A common condition within the knee found in athletes is injury to the anterior cruciate ligament (ACL). The ACL is a ligament that attaches to the tibia and femur. The placement and attachments of the ligament assist in prevention of the tibia translating anteriorly to the femur. The counterpart to the ACL, the posterior cruciate ligament (PCL), has similar attachments but is oriented in a way to prevent the tibia from translating posteriorly on the femur.
The other common injuries to the knee involve the meniscus and the medial collateral ligament (MCL). Each knee is made up of two circular-shaped menisci, which provide structural stability. The MCL attaches the inner portion of the tibia and the femur and functions to resist valgus forces, stressing the knee medially. Located on the outside of the knee, the lateral collateral ligament (LCL) provides similar resistance to prevent varus stress, forcing the knee outward.
There are multiple treatment methods that have been utilized to treat rotator cuff injuries, knee OA and many other orthopedic conditions. More common treatments include pain medication, physical therapy, steroid injection and in some cases surgical intervention.2 Many alternative treatments have been gaining ground in the area of regenerative medicine including PRP and Stem Cell Therapy.
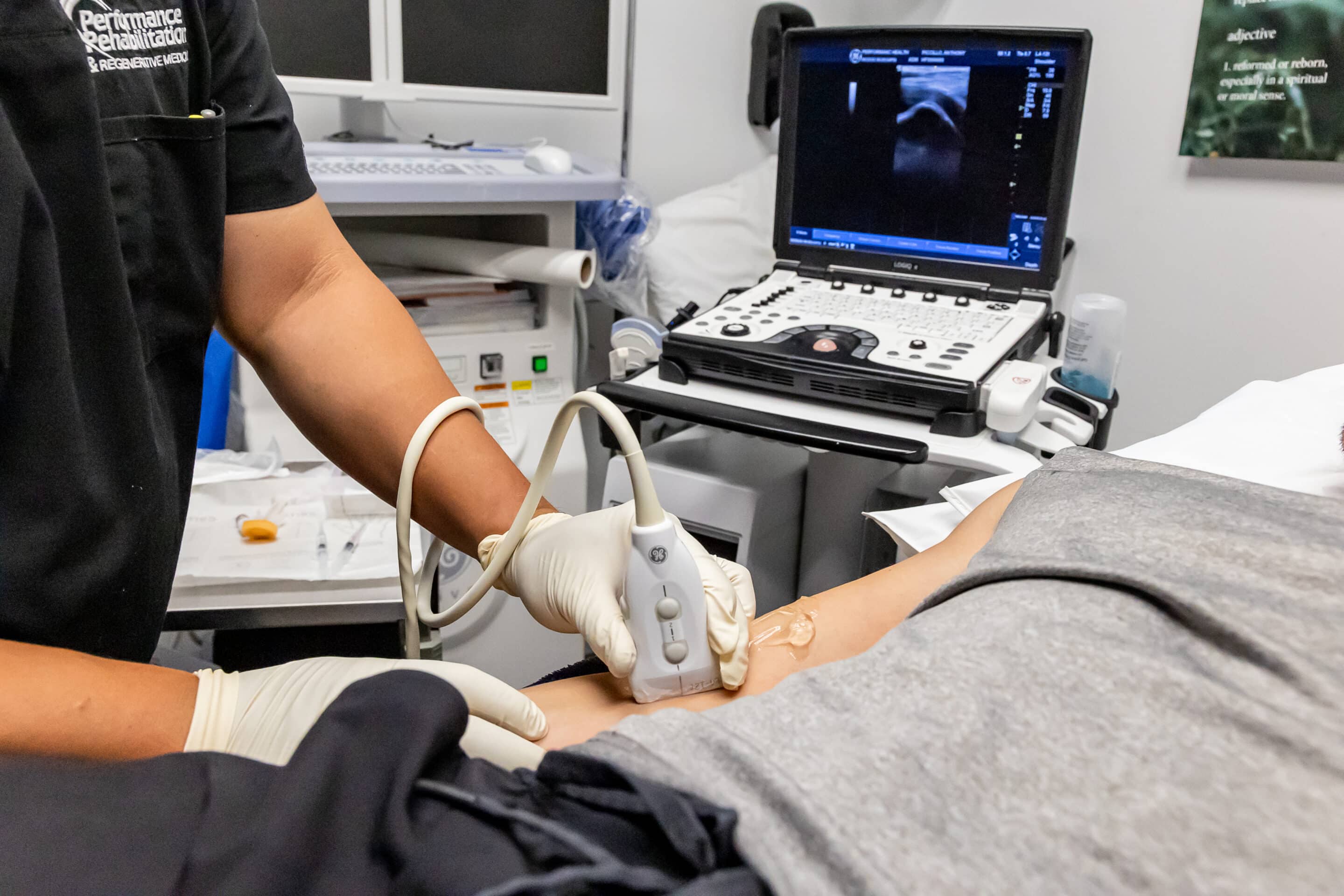
Autologous PRP (meaning from ones own cells) has been used in the treatment of many conditions involving, muscle, tendon, ligament and bone. Because the cells from ones own body are used to target specific areas of injury, PRP has been shown to be a safe and effective means of treatment. Benefits of the treatment include faster recovery time, improved strength, increased range of motion, less pain and decreased inflammation.
Platelets are formed in bone marrow and are the smallest of the blood cells. They contain 30 bioactive proteins, which are vital in tissue healing.3 Growth factor (GF) and the proteins secreted from platelets are understood to have the largest role in tissue healing. GF, specifically Platelet Derived Growth Factor (PDGF), plays a vital role in this process.4 The role of PDGF and other growth factors are not completely understood but have shown to be effective in decreasing healing time and increasing patient outcomes.
The effectiveness of PRP is dependent upon the release of multiple growth factors and how they interact. Platelets are believed to secrete the growth factors within 10-minutes of clotting and more than 95% of all proteins involved in the release within the first hour. Following the initial hour of secretion, additional proteins remain for several days throughout the healing process.5 PRP also contains proteins that act as adhesion molecules. These molecules assist in the healing of many tissue types and promote healing within the targeted area of injury.6
The use of stem cells to promote healing and regeneration in individuals has been an area of great debate, both casually and in federal and local government. A majority of the debate centers on the use of embryonic stem cells. These types of cells are collecting during an organism’s developing stage and have great implications for their application because the cells are able to differentiate into any other human cell. Research has been limited due to the moral and ethical implications.
Alternatively, adult stems hold none of the prior mentioned implications and have shown to be effective in healing many types of tissues. Mesenchymal stem cells specifically are the root cell of bone, cartilage, and muscle tendon and are collected from the adult to which the treatment is performed.
to be effective in healing many types of tissues. Mesenchymal stem cells specifically are the root cell of bone, cartilage, and muscle tendon and are collected from the adult to which the treatment is performed.
In their simplest form, stem cells are an undifferentiated cell that can develop into many types of tissue cells. When the stem cell is applied to a certain type of tissue, it will begin to develop into that same tissue and adhere to the damaged area. This type of technique is called “cell therapy” which allows for the stem cell to differentiate while in contact with its intended tissue type. For example, a collection of stem cells are injected in an area where a muscle tendon is injured. The cells begin to adhere to the healthy tissue and form into tendon tissue in place of the injured or absent tissue.
Stem cells can be collected from many areas of the body but for the use of orthopedic regenerative medicine two sites are most useful. The first is from bone marrow. Cells are collected from long bone, normally the femur, and concentrated into a solution. Alternatively, and often more comfortable to the patient, stem cells can be collected from adipose tissue. The adipose is then placed in a centrifuge and separated into multiple layers. One of the layers becomes concentrated in stem cells and used during the procedure on the same patient.
The use of stem cells in conjunction with PRP has become more common in procedures involving muscles, bones and joints. Because it is a non-surgical procedure and due to lower risk to the individual, these treatments are gaining greater popularity in patients that have failed prior treatments or are looking for an alternative to surgery.
A continuing body of research is developing to support the use of stem cell and PRP therapy for orthopedic conditions. In private practice the procedures are being performed in conjunction with other treatment including physical therapy and have shown to have success. Practitioners that are considering prolotherapy are advised to seek out the most recent literature and guidelines to assist in their clinic decision-making. Continued examination of the outcomes of the procedure is suggested to identify the best treatment options.
If you, or someone you know, are suffering from chronic joint pain, or would like more information on non-surgical orthopedic options, please feel free to contact one of our Physicians at 908-754-1960 or you may contact us online.
About the Authors:
Joseph Mejia D.O., F.A.A.P.M.& R, is a graduate of University of Michigan and West Virginia School of Osteopathic Medicine. He is Board Certified in Physical Medicine & Rehabilitation and Sports Medicine. Dr. Mejia received his Fellowship Training in Interventional Pain Management from University of Medicine and Dentistry. He has advanced training in Regenerative Medicine and is the Medical Director and Partner of Performance Ortho.
John F. Ellis, D.C. is a graduate of Logan Chiropractic College. He is a Board Certified Chiropractic Physician with licenses held in New Jersey and New Hampshire. His past research work involves human performance pertaining to orthopedic conditions. Dr. Ellis is a Chiropractic Physician at Performance Ortho.
References:
- Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost 2004;91:4- 15.
- Grazul-Bilska, A.T., Johnson, M.L., Bilski, J.J., Redmer, D.A., Reynolds, L.P., Abdullah, K.M. Wound healing: The role of growth factors. Drugs Today 2003, 39(10): 787
- Marx RE. Platelet concentrate: a strategy for accelerating and improving bone regeneration. In: Davies JE, ed. Bone engineering. University of Toronto, 2000:447-53.
- Schliephake H. Bone growth factors in maxillofacial skeletal reconstruction. Int J Oral Maxillofac Surg 2002;31:469-84.
- Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-20.
- Bishay V, Gallo RA. The evaluation and treatment of rotator cuff pathology. Prim Care 2013;40:889-910. viii.