What is Degenerative Disc Disease (DDD)?
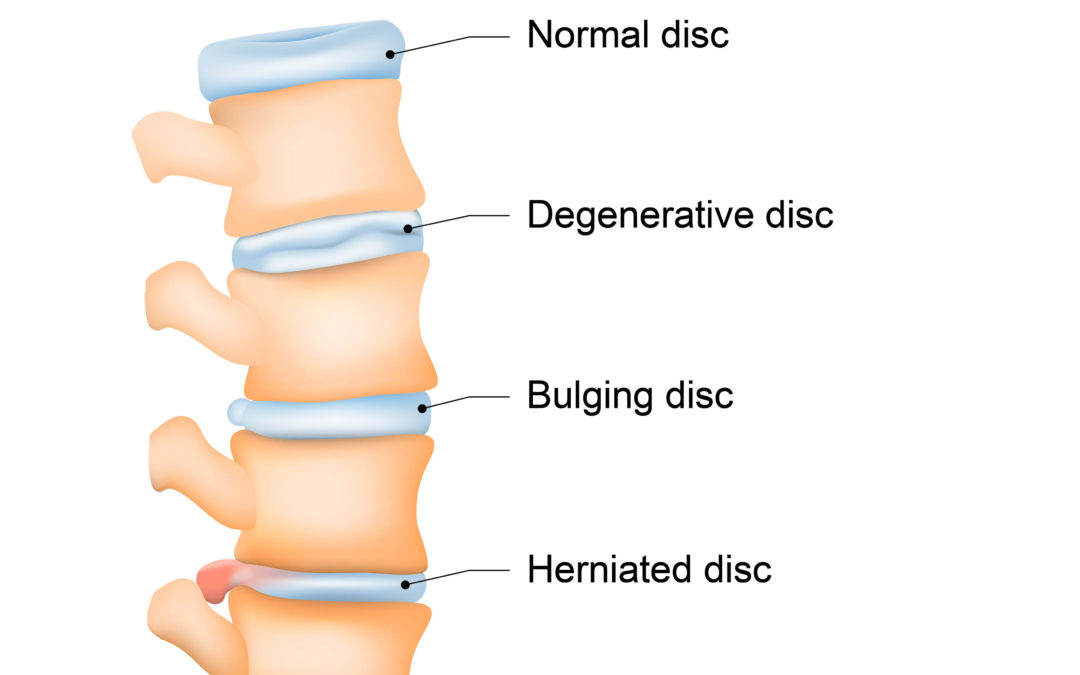
Degenerative disc disease (DDD) is a condition that primarily affects the intervertebral discs in the spine. Contrary to its name, DDD is not actually a disease, but rather a natural part of the aging process for many individuals. The intervertebral discs are cushion-like structures located between the vertebrae of the spine, serving as shock absorbers, and allowing flexibility and movement in the spine.
What causes Degenerative Disc Disease?
Degenerative disc disease (DDD) is characterized by the gradual breakdown of these discs, which can lead to pain, stiffness, and other related symptoms. While the exact cause of DDD isn’t always clear, there are several factors that are believed to contribute to its development:
1. Aging: The primary factor in the development of DDD is the natural aging process. As we age, the intervertebral discs lose some of their water content and elasticity, making them less able to absorb shock and provide proper cushioning between the vertebrae.
2. Genetics: Genetic predisposition can play a role in the development of degenerative disc disease. Some people may have a genetic makeup that makes their discs more susceptible to degeneration.
3. Trauma or Injury: Previous injuries to the spine, such as fractures or accidents, can accelerate the degenerative process of the intervertebral discs.
4. Repetitive Strain: Engaging in activities that place repetitive strain on the spine, such as heavy lifting, bending, or twisting, can contribute to disc degeneration over time.
5. Poor Posture: Consistently maintaining poor posture, such as slouching while sitting, can place uneven stress on the intervertebral discs and contribute to their degeneration.
6. Smoking: Smoking has been linked to increased disc degeneration. It can impair blood flow to the discs, reducing their ability to receive nutrients and oxygen.
7. Obesity: Excess weight places added stress on the spine, which can contribute to disc degeneration.
8. Lack of Physical Activity: A sedentary lifestyle can weaken the muscles that support the spine and decrease the flow of nutrients to the discs, potentially accelerating degeneration.
9. Inflammation: Chronic inflammation can contribute to disc degeneration by damaging the tissues of the disc and surrounding structures.
10. Medical Conditions: Certain medical conditions, such as rheumatoid arthritis or ankylosing spondylitis, can increase the risk of degenerative disc disease.
It’s important to note that degenerative disc disease is a complex condition, often resulting from a combination of these factors. While the degenerative process is a natural part of aging, adopting a healthy lifestyle, practicing good posture, maintaining a healthy weight, and avoiding excessive strain on the spine can help reduce the risk of developing or worsening degenerative disc disease.
What are the symptoms of Degenerative Disc Disease?
Why does my back feel like it is popping?
The most common symptom associated with degenerative disc disease is chronic low back pain. This pain can vary in intensity and may worsen with movement, lifting, or prolonged sitting or standing. The pain may radiate into the buttocks and legs if nerves become compressed or irritated due to disc changes. Other symptoms can include numbness, tingling, or weakness in the legs. The symptoms of degenerative disc disease can vary from person to person, but commonly include:
1. Pain: The most common symptom is chronic, low-grade back pain. The pain might be localized to the affected disc or radiate to nearby areas, such as the buttocks, hips, thighs, or even down into the legs (sciatica). The pain can be aggravated by certain movements, such as bending, lifting, or twisting.
2. Stiffness: You might experience stiffness in the morning or after prolonged periods of inactivity. This stiffness usually improves as you move and become more active.
3. Pain with Movement: Activities like bending, lifting, or twisting might exacerbate the pain. Certain positions or movements can put extra stress on the degenerated discs, leading to discomfort.
4. Numbness and Tingling: If a degenerated disc is compressing a nerve root, you might experience numbness, tingling, or a sensation of pins and needles in the affected area. This is particularly common when a nerve root irritation leads to sciatica.
5. Weakness: In some cases, nerve compression due to degenerative disc disease can lead to muscle weakness in the affected region. This weakness can affect your ability to perform certain activities and maintain balance.
6. Pain Relief with Rest: Resting or changing positions might alleviate the pain. People with DDD often find relief when they lie down or change their posture, taking the pressure off the affected discs.
7. Pain Flare-ups: Periods of relatively low pain might be interspersed with flare-ups where the pain becomes more intense. These flare-ups can be triggered by activities or movements that stress the affected discs.
It’s important to note that not everyone with degenerative disc changes experiences pain or discomfort. Additionally, the term “degenerative” can sometimes be misleading, as it implies a disease process, when in reality, these changes are a normal part of the aging spine for many people.
How do you diagnose Degenerative Disc Disease?
Diagnosis of degenerative disc disease typically involves a combination of medical history, physical examination, and imaging studies (such as X-rays, MRI, or CT scans) to assess the condition of the discs and rule out other potential causes of symptoms.
1. Loss of Disc Height: The discs lose water content over time, causing them to become thinner and reducing the space between vertebrae.
2. Changes in Disc Composition: The composition of the discs can change, with a decrease in proteoglycan content (substances that help retain water) and an increase in collagen content (making the discs less flexible).
3. Cracks and Tears: The outer layer of the disc, known as the annulus fibrosus, can develop cracks or tears, potentially leading to the leakage of inner disc material.
4. Bone Spurs: The body may respond to disc degeneration by forming bony growths (osteophytes) around the edges of the vertebrae, which can contribute to spinal instability and nerve compression.
5. Reduced Shock Absorption: Degenerated discs are less effective at absorbing shock and distributing forces during movement, leading to increased stress on surrounding structures.
Treatment Options for Degenerative Disc Disease in New Jersey
How do you treat Degenerative Disc Disease?
Treatment for degenerative disc disease focuses on managing pain, improving function, and enhancing quality of life through a combination of conservative measures, pain management techniques, and, in severe cases, surgical intervention.
The treatment for degenerative disc disease (DDD) can vary based on the severity of symptoms, the patient’s overall health, and other individual factors. The goal of treatment is typically to manage pain, improve function, and enhance the patient’s quality of life. Here are some common treatment options at Performance Rehabilitation for DDD:
– Physical Therapy: A physical therapist can develop a tailored exercise program to strengthen the muscles that support the spine, improve flexibility, and promote better posture.
– Epidural Steroid Injections: These injections can provide temporary relief by reducing inflammation and pain around the affected disc.
– Nerve Block Injections: These injections target specific nerves to block pain signals from reaching the brain.
– Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body and may help alleviate pain for some individuals.
– Platelet-Rich Plasma (PRP) Therapy: PRP involves injecting a patient’s own concentrated platelets to promote healing and reduce inflammation.
– Stem Cell Therapy: Stem cells can be used to stimulate tissue repair and potentially slow down the degenerative process.
– Chiropractic Care: Some individuals find relief through spinal manipulation performed by trained chiropractors.
– Microdiscectomy: This minimally invasive surgery involves removing a portion of the damaged disc that might be pressing on a nerve and causing pain.
– Laminectomy: In this procedure, a part of the vertebral bone (lamina) is removed to relieve pressure on the spinal cord and nerves.
– Spinal Fusion:*This procedure involves fusing two or more vertebrae together to stabilize the spine. It may be recommended if DDD has led to spinal instability.
– Artificial Disc Replacement: In select cases, a damaged disc can be replaced with an artificial one, preserving spinal motion.
Treatment recommendations should always be tailored to an individual’s specific needs and guided by healthcare professionals. A comprehensive approach that combines conservative measures, pain management, and surgical options when necessary can help effectively manage the symptoms and progression of degenerative disc disease. Give us a call today to book a consultation and stop living with back pain, at 908-274-1011 or click to book an appointment.
Visit any of our 3 locations in Branchburg, NJ, Somerset, NJ, Watchung, NJ or our Surgical Center in Bridgewater, NJ.